Total nucleated cell (TNC) and mesenchymal stem cell (MSC) counts – what is the difference?
When patients come to Regenexx Cayman for stem cell treatment, they are often curious about which metrics we use to assess the quality of their marrow sample. What specific cell counts do we take? What do these counts mean, and how do they compare between patients? To understand the difference between total nucleated cell (TNC) and mesenchymal stem cell (MSC) counts, let us first consider the many different cell types present within bone marrow.
First, bone marrow contains hematopoietic stem cells (HSC) that give rise to all of the body’s blood cells – this includes a complex lineage of white blood cells that ultimately make up your immune system, as well as red blood cells that travel through your circulation and deliver oxygen to your tissues (see Figure 1). Hematopoietic stem cells in the marrow give rise to progenitor cells, a type of intermediate precursor cell, which then travel in the blood and lymphatic systems and mature into functional immune cells such as T cells, antibody-secreting memory B cells, natural killer (NK) cells, and macrophages.
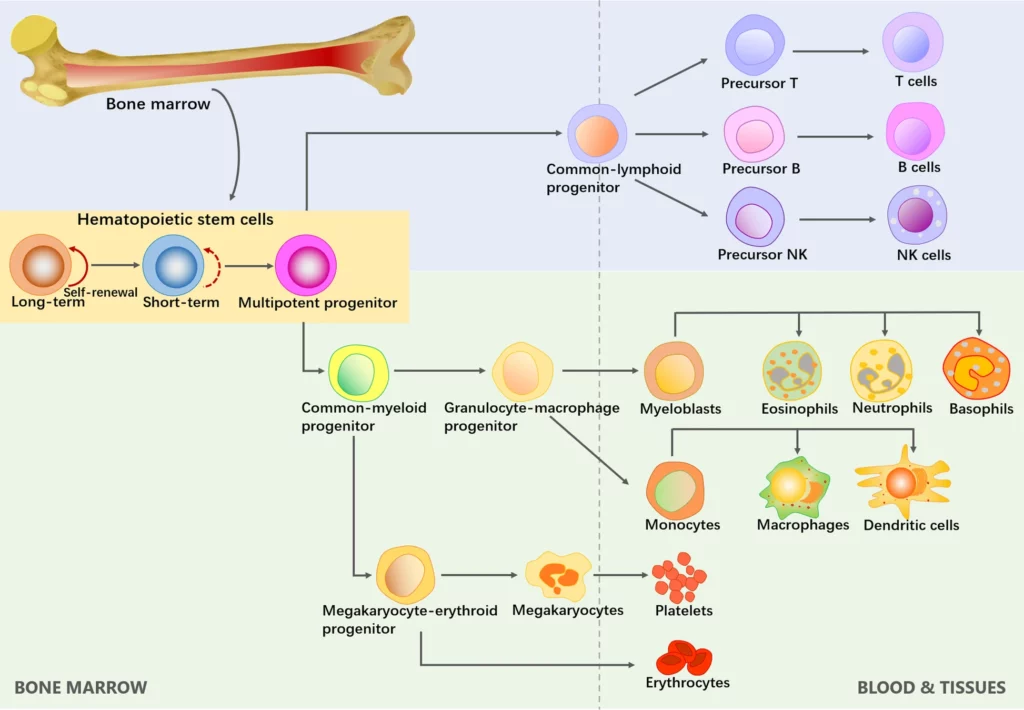
Separate from the hematopoietic cell lineage, bone marrow also contains a very small fraction of mesenchymal stem cells (MSC). These are adult stem cells that are important for repairing connective tissues such as muscle, bone, fat, and cartilage. Mesenchymal stem cells account for ~0.001–0.01% of bone marrow nucleated cells (Bhat et al., 2021; Kim et al., 2020). For example, a total nucleated cell count (TNC) of 1 billion contains somewhere in the range of 10,000 – 100,000 MSC.
While comprising a seemingly small fraction of the total cell count, we know that MSC play an important role in regulating tissue repair. Therapeutic benefits of MSC are attributed to:
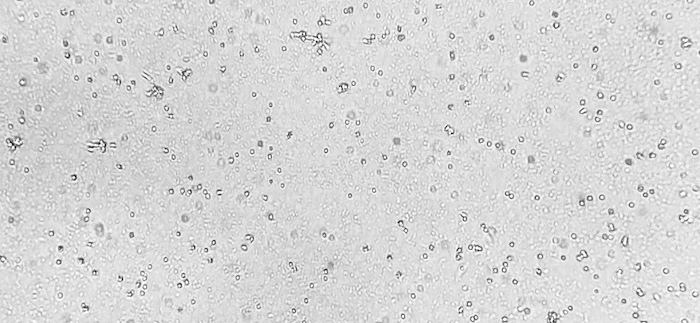
Importantly, MSC also have the capacity for self-renewal, which is the ability to replicate and create identical daughter cells. Because of this capacity for self-renewal, we can isolate that small 0.001-0.01% fraction of MSC from bone marrow and expand these cells in culture to much greater numbers than you would find in the body (see Figure 2, Figure 3).
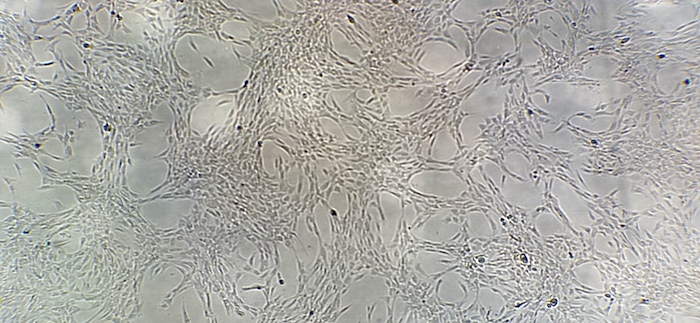
From this expanded yield of stem cells, we are able to harvest and cryopreserve a bank of frozen cells for future treatments. We can thaw and further expand cells as needed to prepare high-dose stem cell injections, known as Regenexx-C.
To say it another way – marrow contains a mixture of cell types. Some of these cells do not have a nucleus. Generally, red blood cells do not have a nucleus. Red blood cells are biconcave disc-shaped cells, small by design, allowing them to travel through small veins and capillaries. Platelets are small cell fragments that do not have a nucleus. Excluding red blood cells and platelets that do not have a nucleus, TNC measures the starting number of nucleated cells in a sample of bone marrow concentrate. These are cells with a nucleus, a copy of the genome, and the cellular machinery required for gene expression. Within this population of nucleated cells, mesenchymal stem cells (MSC) make up less than one percent, but this small fraction of MSC can be isolated and culture-expanded in our advanced laboratory.
Not always, but generally, the nucleated cell count at time of marrow aspiration correlates with final MSC yield after cell culture expansion. More nucleated cells to begin with means more colony-forming, replicating stem cells to expand over time in culture. Nucleated cell counts vary between patients, and even between different marrow samples from the same patient. These differences can be due to age, gender, overall health and underlying conditions, volume of marrow aspirated, and marrow sample composition. While it is natural to be curious how your numbers compare to other patients, the absolute cell counts are less important than the manyfold increase in cell number achieved through culture expansion, relative to your original sample.
Cultured cell treatments are based on speeding up the body’s healing process. Compared to the body’s physiological “1X” response, which involves cells naturally mobilizing from the bone marrow and traveling to the site of an injury, cell culture allows us to accelerate the process by taking those same cells, expanding them to large numbers, and injecting a concentrated dose precisely where they are needed.
In summary:
Written by Chase Demarest, Lab Manager at Regenexx Cayman.
References