Hip arthritis is a debilitating condition that affects millions of people worldwide. As we age, the cartilage in our hip joints can deteriorate, leading to pain, stiffness, and reduced mobility. While traditional treatments, such as physical therapy, medications, and surgery have been the go-to options, a promising alternative has emerged: the use of culture-expanded Mesenchymal Stem Cells (MSCs).
Today, we will explore how MSCs are changing the landscape of hip arthritis treatment and discuss how this treatment has helped a recent triathlete!
Understanding Hip Arthritis
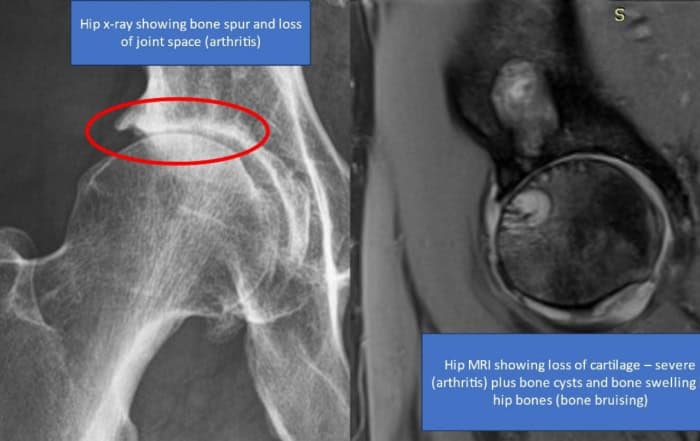
Before delving into MSC therapy, it’s crucial to understand what hip arthritis is. Hip arthritis, also known as hip osteoarthritis, is a degenerative joint disease that occurs when the protective cartilage in the hip joint breaks down over time. This can lead to friction, pain, inflammation, and ultimately, joint damage. Patients often experience difficulty walking, climbing stairs, and performing everyday tasks.
Recent studies have shown that hip arthritis is much more than just a breakdown of cartilage. While many people have loss of cartilage, long-term research says that loss of cartilage alone is NOT a predictor of hip pain! An analysis of the Framingham study data showed that among more than 700 patients, the loss of cartilage on MRI was not associated with pain.
Is Your Hip Arthritis Getting Worse Due to a BML?
We used to believe that the degree of arthritis, or cartilage degeneration, was associated with pain (i.e., more arthritis equals more pain), but research has dispelled this urban myth. One of the few MRI findings that has withstood the test of time and many different research studies as being related to pain is a BML (bone marrow lesion).
A bone marrow lesion is an area in the bone that’s swollen. Basically, it’s the bone’s reaction to bad cartilage or the excessive forces due to instability, and as mentioned above, BMLs are also associated with microscopic fractures in the bone. BMLs are basically a microscopic stress fracture in the bone. For lack of a better term, BMLs are “pissed off bone.”
A recent study shows that bigger BMLs at the start of the study (also called BMEs), were associated with hip arthritis getting worse (i.e., more hip pain) and poorer quality of life as the study progressed. This is consistent with other studies correlating BMLs with hip pain. For example, this study published in Clinical Rheumatology stated, “Cross-sectionally, the presence of large femoral, acetabular, or any hip BMLs was associated with higher odds of hip pain…High cartilage signal was strongly associated with hip BMLs, but not with pain.”
Is Hip Arthritis Harder to Treat compared to Other Joints?
Our registry data shows that, on average, patients with severe hip osteoarthritis (OA) don’t respond as well to a same-day bone marrow concentrate (Regenexx-SD) procedures as those with severe knee OA.
Interestingly, hips have fewer native stem cells than knees (i.e., hips lack the same self-repair mechanism as knees, and research shows hip and knee arthritis are different diseases). Hips can also have much more rapid bone changes on MRI than knees. In fact, a hip can deteriorate within a year, while knees can smolder for many years.
This explains why our registry data also shows significantly better improvement with Regenexx-C for hip arthritis as compared to Regenexx-SD – a higher number of cells = better improvements. For instance, 18 months after Regenexx-C treatment, hip patients reported an overall improvement of 50%. Two years after Regenexx-C treatment, they reported a pain score of only 1.5/10 and a functional improvement of 91%.
The Role of Mesenchymal Stem Cells (MSCs)
Mesenchymal Stem Cells, or MSCs, are multipotent cells found in various tissues throughout the body, including bone marrow and adipose tissue. These cells have the remarkable ability to differentiate into different cell types, including cartilage, bone, and fat cells. This regenerative potential makes MSCs an attractive option for treating conditions like hip arthritis.
Culture-Expanded MSC Therapy
Culture-expanded MSC therapy involves the isolation of MSCs from a patient’s own body. Taking your own cells is referred to “autologous,” which means it’s from you, going back into you! With the help of our cell biologists, these cells are then cultured in a lab to increase their numbers. Typically, the baseline numbers are increased to 100 to 1,000 – fold increase!
Once an adequate quantity is obtained, the cultured MSCs are injected directly into the affected hip joint. With hip arthritis we aim at not only treating the cartilage loss, but, more importantly, we utilize x-ray guidance to place cells directly into the bone – targeting the BMLs. This is targeting the main pain generators in the hip as well.
Here’s how this therapy can help in the treatment of hip arthritis:
Clinical Case:
Meet: AL – a 52y/o triathlete who, unfortunately, was born with hip dysplasia but did not let that slow her down in her pursuit of athletics! When a hip replacement would all but guarantee an end to her triathlete days, she turned to Regenexx-C and Dr. Pitts for help in allowing her to continue running and athletics.
As discussed above, her MRI showed a big reason for her hip pain. Having a significant amount of sub-chondral edema and BMLs in addition to large cysts in her bone.
AL was treated in early 2023 – treatment consisted of autologous cultured stem cells, whereby cells were placed with extreme precision using both ultrasound guidance and live x-ray guidance to place the cells into the hip joint, ligaments around the hip, and directly into the damaged bone!
Here is the 4-month check in after the procedure:
“AL is following up about 4 months post-Cayman treatment in January. She is doing great. Her range of motion has improved. It is maybe about 85% in flexion of the left hip. She has been doing PT twice a week. Her stability of the hip feels much better. She does not get that feeling like it is going to cut out the socket anymore. She has been working her way up on antigravity treadmill to start at 70% body weight up to 80% body weight. Swimming and bike did not bother her and still do not. She used to be wiped out after doing any running like that, but now she may get a little stiffness afterwards, but nothing like before. She can run about 10-11 minute mile pace. She has a race plan for July. It is a 10K, which she will decide in a couple of weeks if she will just cut off the running portion or do a shorter distance just to see. Seems like she is progressing slow and steady, listening to her body, but things are going very well, especially considering.”
August update:
Her race in July went well without much of an issue and AL continues to. Being 8-9 months out from procedure and starting to run longer and longer distances is great and couldn’t be happier with her success!
Conclusion
Culture-expanded MSC therapy represents an exciting development in the field of hip arthritis treatment. It represents the most advanced ortho-biology in the world: the ability to use purified and expanded (100-1,000x) stem cells from your own body. As research continues to advance, we may witness even more significant breakthroughs in this area, offering hope to those living with this challenging condition.
Written by Dr. Jason Markle.